
- ● Lifestyle Factors Driving Gut Imbalances
- ● Dysbiosis, PAMPs, Systemic Inflammation, and Chronic Diseases
- ● Evolutionary Mismatch and Holistic Interventions
- ● Why Root-Cause Healing Was Forgotten? How We Forgot to Prefer Pills over Lifestyle?
- ● How Can the Ancestra Health App Help?
- ● Apply for Free Early Access Membership
Modern Lifestyle, Chronic Diseases, and the Ancestra Health App
15 min read ● by Ancestra Health Research
● Lifestyle Factors Driving Gut Imbalances
Gut-related issues are the most significant contributors to the continuously growing chronic disease epidemic. Modern living exposes our gut to many disruptive factors. A high-carbohydrate diet rich in ultra-processed foods fosters dysbiosis, an unhealthy, imbalanced gut microbiome. Refined carbohydrates, especially simple sugars, are rapidly absorbed and offer little fuel for beneficial gut microbes, which allows potentially pathogenic microbes to proliferate and become pathogenic[*]. In contrast, for example, collagen-rich animal foods can support microbial fermentation and gut homeostasis[*][*]. Chemical food additives (emulsifiers, artificial sweeteners, colorants, preservatives) common in processed foods further impair gut health. They can alter the microbiome, thin the protective mucus layer, damage the intestinal barrier, and trigger abnormal immune reactions[*][*]. Food components, such as meat, collagen, or low-starch vegetables, are not consumed in adequate quantities to achieve a high enough GLP-1 response, which could slow sugar uptake and prevent dysbiosis from occurring [*][*][*][*]. Frequent snacking leaves little time for the gut’s cleanup waves between meals, potentially promoting bacterial overgrowth. Chronic stress is another culprit, as it exacerbates the problems caused by poor-quality food[*]. Circadian disruption, characterized by irregular sleep patterns, late-night screen exposure, and shift work, also affects gut balance. Our bodies evolved in response to daily light/dark cycles, and modern lighting can disrupt microbial rhythms and metabolism[*][*][*]. Lastly, chemical exposures weaken the gut ecosystem. Residual agrochemicals (like certain pesticides) in food can kill beneficial microbes or favor hardy pathogens[*]. The overuse of antibiotics[*][*] or other drugs (e.g., NSAIDs[*][*], antacids[*]) can wipe out friendly gut bacteria and inflame the gut lining. In combination, these lifestyle factors create a “perfect storm” for gut imbalance.
● Dysbiosis, PAMPs, Systemic Inflammation, and Chronic Diseases
An imbalanced gut (dysbiosis) sets off a chain reaction of immune stress. Harmful bacteria overgrow and release PAMPs (pathogen-associated molecular patterns), for example, lipopolysaccharide (LPS), a toxin from Gram-negative bacterial cell walls. A healthy intestinal barrier normally blocks these, but dysbiosis plus a “leaky gut” allows such microbial fragments to translocate into the bloodstream[*]. The immune system reacts as if under chronic attack, mounting persistent inflammation throughout the body. This silent inflammation originating in the gut can disrupt metabolism and organ function. For instance, after a high-carbohydrate, processed meal in a Western diet, LPS levels in the blood can spike and trigger inflammatory signaling via Toll-like receptor 4 (TLR4). Over time, this contributes to mitochondrial dysfunction (our cells’ energy powerhouses falter under oxidative and inflammatory stress) and insulin resistance (cells respond poorly to insulin due to inflammatory signaling). These changes underlie many chronic diseases. Indeed, metabolic endotoxemia from dysbiosis has been implicated, for example, in autism, Alzheimer’s disease, Parkinson’s disease, arthritis, obesity-induced osteoarthritis, and asthma[*]. Systemic inflammation and altered immunity can also provoke autoimmune conditions. Dysbiosis is associated with immune-mediated diseases, including rheumatoid arthritis, type 1 diabetes, multiple sclerosis, and lupus [*]. The brain is not spared either: inflammatory molecules and even bacteria from a leaky gut may affect the brain’s immune cells and neurotransmitters, contributing to mental disorders like depression and anxiety in susceptible individuals[*]. Researchers have coined the term “gut-brain axis” to describe this intimate connection; for example, gut dysbiosis has been associated with higher rates of depression, autism, and schizophrenia, likely via chronic inflammation and altered neurochemicals[*]. In sum, an imbalanced gut can chronically activate the immune system and derail metabolism, eventually manifesting as diseases ranging from obesity, hypertension, and heart disease to autoimmune and neuropsychiatric disorders. Many of these modern illnesses thus share common roots in chronic inflammation and metabolic dysfunction driven by gut-derived signals.
● Evolutionary Mismatch and Holistic Interventions
Why are these chronic conditions so widespread now? An evolutionary mismatch exists between our Stone Age biology and the modern world. For almost two million years, humans lived as hunter-gatherers, and our bodies adapted to that environment. Our Paleolithic ancestors consumed whole foods, typically low in carbohydrates and high in meat and fat[*], and experienced periods of feast and famine. They were exposed to natural light patterns and engaged in regular physical activity. Today, we inhabit a completely different reality of 24/7 food availability, processed high-carb diets, indoor living, and inactivity. This mismatch is driving the epidemics of chronic disease. Early hunter-gatherers (and modern indigenous groups living traditionally) avoided the diseases of civilization. They didn’t suffer from obesity, diabetes, heart disease, etc. In some environments, ancestral diets were very low in carbohydrates: for example, Arctic Inuit traditionally derived basically all of their calories from fatty meat (marine animals), with minimal plant food[*]. In most climates, our ancestors ate plenty of protein and fibrous plants but no refined grains or sugars. They experienced natural light-dark cycles (bright days, dark nights) and maintained robust circadian rhythms; there was no artificial light to disrupt sleep or hormones. They fasted intermittently, not by choice but because food wasn’t constantly at hand – this gave their bodies time to rest, repair, and regulate metabolism between meals. And importantly, they moved their bodies daily – foraging, hunting, climbing, digging – far from the sedentary desk-bound lives many lead now. As Harvard evolutionary biologist Daniel Lieberman puts it, we are creatures designed for a world that no longer exists[*]. The result of this discordance is a surge in “mismatch diseases” like type 2 diabetes, atherosclerosis, and even cancers that our ancestors didn’t encounter.The good news is that aligning our lifestyle more closely with our evolutionary heritage can restore balance in most cases. Holistic interventions that address the root causes by mirroring key aspects of ancestral life provide solutions to most modern diseases. Adopting a lower-carbohydrate diet of whole, unprocessed foods, adding more animal-based components, and natural fats can reverse dysbiotic microbes and nurture a healthy microbiome, reducing inflammation. Different versions of this diet can address various health issues[*]. If needed, incorporating periodic fasting or longer gaps between meals gives the gut time to reset and improves insulin sensitivity. Ensuring exposure to natural light (especially morning sunlight) and minimizing artificial light at night helps recalibrate our circadian clock, benefiting metabolism and immune function[*]. Simply put, sleeping when it’s dark and being active when it’s light is deeply in tune with our biology. Regular physical activity is also critical: Our body responds to low physical activity by decreasing our muscle and bone mass. Exercise not only burns calories but also triggers anti-inflammatory effects and even promotes a diverse gut microbiome. Even moderate activity (like walking, lifting, or playing) done consistently can mimic the active lifestyle our genes are geared for and protect against chronic disease[*]. Finally, managing stress and allowing time for rest is part of an ancestral pattern that we often forget – our forebears experienced intense physical stresses but also periods of recovery, whereas modern psychological stress is often unrelenting. Mind-body practices, time spent in nature, and adequate downtime can help lower chronic cortisol levels and promote healing of the gut-immune axis. By addressing nutrition, movement, light, and stress in tandem – an approach our Paleolithic ancestors implicitly followed – we tackle the root imbalances. Many people who adopt these lifestyle changes experience improvements in blood sugar, blood pressure, weight, and inflammation markers, illustrating the body’s remarkable capacity to heal when returned to a more natural regimen.
● Why Root-Cause Healing Was Forgotten? How We Forgot to Prefer Lifestyle over Pills?
If the benefits of lifestyle changes are so clear, why aren’t they front and center? Unfortunately, several systemic factors have conditioned society to favor pills and procedures over prevention. Medical education itself has historically neglected nutrition and lifestyle. Until recently, doctors-in-training received only a few hours of nutrition coursework on average, with little emphasis on behavior change or preventive care [*]. As one physician noted, this paucity of lifestyle training is part of “a legacy of a treatment model based on pharmacology and surgery,” rather than root-cause healing. The pharmaceutical industry reinforces this bias. The business of medicine is reactive mainly. Vast sums are spent marketing drugs and high-tech interventions. Pharmaceutical companies aggressively promote their products to both doctors and the public. In fact, about 90% of pharma’s marketing budget is directed at influencing physicians (through sales reps, sponsored education, free samples), and studies show that doctors who receive industry payments tend to prescribe more brand-name and unnecessary medications[*]. Meanwhile, consumers are bombarded with direct-to-consumer drug ads and messages that there’s “a pill for every ill.” Mainstream dietary guidelines and food marketing have also sown confusion. Past guidelines promoted grain-centric, high-carbohydrate diets (partly due to industry lobbying), normalizing the very eating patterns that cause the diseases. For example, in the 1960s, the sugar industry paid scientists to blame fats for heart disease instead of sugar, distorting public nutrition policies for decades[*]. To this day, big food companies fund research that often (not surprisingly) finds processed foods or sweet drinks to be benign, muddying the waters of public advice[*]. This siloed and profit-driven approach in healthcare tends to compartmentalize problems (treating symptoms organ by organ) and dismiss holistic or integrative treatments as unscientific. A doctor might treat an autoimmune disease with immune-suppressing drugs, for instance, without addressing the patient’s diet, stress, or gut health that underlie the immune imbalance. Likewise, someone with depression might get an antidepressant, but no discussion about replacing the inflammatory diet with nutrition that heals. The result is a populace conditioned to seek quick fixes and view chronic issues as isolated ailments rather than symptoms of lifestyle imbalance. Over the years, we’ve been “brainwashed” to accept that managing disease is about prescriptions and surgeries, while prevention or reversal through lifestyle sounds too extreme. Challenging this narrative requires unlearning many of the assumptions the media, industry, and even well-meaning professionals have instilled in us.
● How Can the Ancestra Health App Help?
Ancestra Health aims to put the power and responsibility back in your hands. Our app is built on the root-cause, scientific, evolution-based approach to healing from noncommunicable chronic diseases, acting as a personal guide to realign your lifestyle with what your body naturally needs. Instead of a top-down “take this pill” directive, the app empowers users through education and personalized coaching. It helps you understand how factors like diet, sleep, sun exposure, and exercise are affecting your unique physiology. Using input you provide (on your eating habits, symptoms, lab results, etc.), it identifies the likely root imbalances, be it a dysbiotic gut, chronically high blood sugar, or disrupted circadian rhythm, and then offers tailored, practical steps to address them. You will have the freedom to select action items that are compatible with you. For example, Ancestra Health might discover that your diet is high in glycemic processed carbs and coach you to gradually transition to a lower-carb, nutrient-dense meal plan that can heal your diseases. It could suggest a time-restricted feeding schedule to normalize insulin rhythms, guide you in meditation techniques to tame stress (thereby also improving leaky gut), or remind you to get morning sunlight and dim lights at night to fix a circadian glitch. Throughout, the focus is on lifestyle as medicine. The app leverages cutting-edge science to demonstrate that with the right lifestyle changes, the body can repair itself, restoring a healthy gut and metabolism, calming inflammation, and reversing or at least mitigating diseases. You can choose symptoms and lab tests to track your progress to healing. Seeing these wins reinforces the truth that, unless irreversible damage has happened, our bodies can heal when given the chance. Ancestra Health’s approach counters the passive patient mindset; you become an active participant in your healing journey. Importantly, the app fosters consistency. It keeps you motivated with reminders and shows your progress using charts. By aligning lifestyle to our ancestral biology, the app helps reverse the root causes of illness – not by magic, but by harnessing the same self-healing mechanisms that kept our ancestors robust. The best doctor is your own body, when supported by the proper habits. With knowledge, encouragement, and personalized strategies, the Ancestra Health app puts the power of holistic health back where it belongs – with you.
● Apply for Free Early Access Membership
Ancestra Health is inviting individuals with chronic health conditions to participate in our value-packed Early Access Membership program at no cost.
This special Early Access Membership includes the following free benefits for our 6-month program:
✓ app subscription
✓ weekly supervision
✓ lab tests
We regularly publish science-backed health articles in our blog. If you don’t want to miss any, please subscribe to our newsletter.
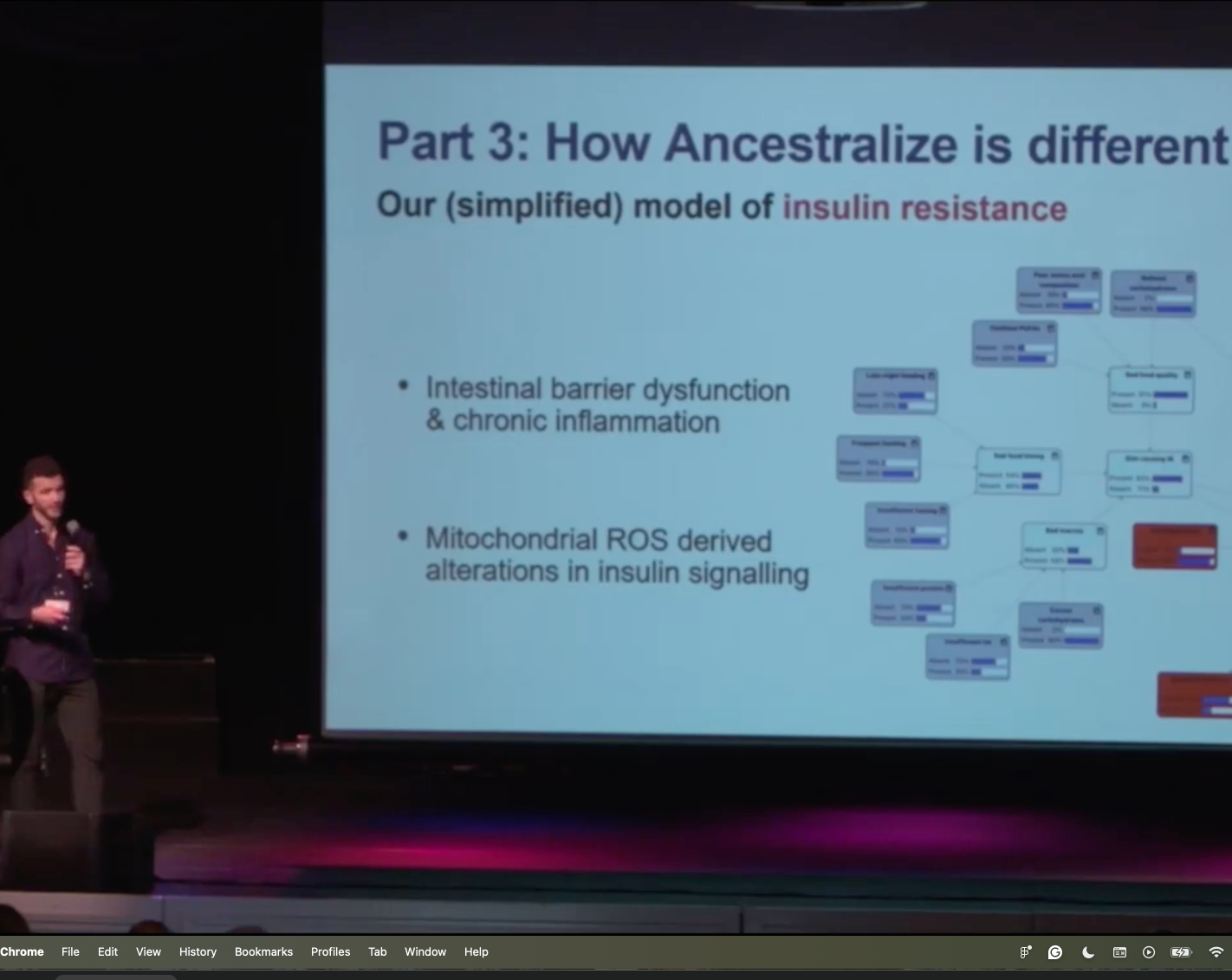
The video recording of our colleague Raphael Sirtoli’s presentation at the CoSci Conference 2024, about our pre-launch app


